Scrotoplasty in Gender-Affirming Surgery
Scrotoplasty is a gender-affirming surgery that involves creating or reconstructing a scrotum, using tissue from the labia majora. The final appearance, size, and position of the scrotum can vary depending on each individual’s anatomy. Testicular implants are usually added during a later stage of the surgical process.
Hoebeke’s Technique
Hoebeke’s Technique—commonly known in the trans community as V-Y Scrotoplasty and sometimes referred to by surgeons as Ghent-style scrotoplasty—is the most widely used method for creating a scrotum during gender-affirming bottom surgery. Developed by Professor Piet Hoebeke and his team at Ghent University Hospital in Belgium, the technique was first detailed in the landmark 2009 publication, "Scrotal Reconstruction in Female-to-Male Transsexuals: A Novel Scrotoplasty."
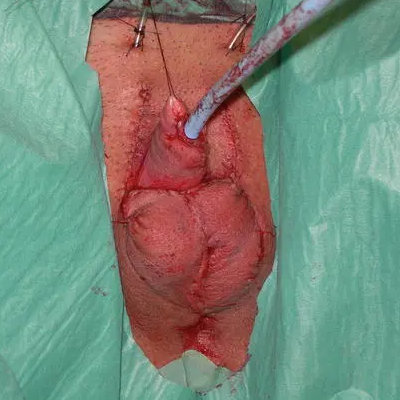
This technique uses the labia majora to create a natural-looking scrotum. The term “V-Y” refers to the surgical flap design: each labium is incised in a V-shape, then the tissue is carefully dissected, rotated inward, bent on itself, and closed in a Y-shape. These flaps form the two halves of the scrotum, which are sutured together at the midline and anchored forward so that the new scrotum sits in front of the thighs.
Hage's VY-Scrotoplasty
Hoebeke’s Technique builds on an earlier method of scrotoplasty that also used V-Y advancement of the labial skin. First described in 1993 by Hage et al., that approach often resulted in a scrotum positioned between the legs. To address this, Hoebeke and his team introduced key refinements: rather than simply advancing the labial flaps, they rotated and folded them inward to form a more rounded scrotum that sits in front of the legs, more closely resembling cis male anatomy. They also incorporated skin from the clitoral area to improve the appearance and texture of the scrotum. Another major goal of the updated technique was to preserve sensation. By carefully preserving tissue and nerve pathways, the procedure helps maintain both tactile and erogenous sensitivity in many patients. Overall, these innovations were driven by patient feedback and aimed at producing a more natural-looking result.

Belgrade Scrotoplasty
Implants and Staging
In most cases, testicular implants are not placed during the initial scrotoplasty. Surgeons typically wait 6 to 12 months to allow the newly constructed scrotum to heal fully before placing implants.
One exception is the Belgrade metoidioplasty, which is performed as a single-stage procedure and includes immediate placement of testicular implants. However, this approach does not use the V-Y scrotoplasty technique. Instead, it involves a different method that results in a more visibly separated, or bifid, scrotum.
Yes. Dr. Gabriel Del Corral discusses a technique using Z-plasty to reduce bifidity and improve scrotal appearance. Please note: The video contains graphic surgical content.
- Watch his explanation here: Watch Video
Keep in mind: if implants are already in place, they must be removed before the revision, then replaced in a second surgery 6 to 12 months later.
For patients receiving an inflatable erectile device (following phalloplasty), the internal pump is typically placed in one side of the scrotum, with a single testicular implant placed in the other.
Tissue Expansion for Larger Scrotal Implants
In some cases, tissue expanders are used to gradually stretch the labial tissue, making room for larger testicular implants. This approach is particularly helpful when there isn’t enough tissue available to create a sufficiently sized scrotum. Instead of placing implants immediately, surgeons insert saline-filled tissue expanders, which are slowly inflated over a period of four to six months. This gradual stretching increases the volume of the scrotal pouch and prepares it for the eventual placement of larger implants.
Once the desired expansion is achieved, a second surgery is performed to remove the expanders and insert permanent testicular implants.
While this method can be effective, it comes with drawbacks. The expansion process can be uncomfortable or painful, and it adds another surgical stage. However, for patients with limited labial tissue, it may offer long-term benefits by enabling a more proportional scrotum.
There are few published reports on the use of tissue expanders in transgender men, and the technique is relatively uncommon. According to Dr. Mang Chen, the practice has largely fallen out of favor. He recommends an alternative strategy known as passive tissue expansion, where small testicular implants are placed first, then replaced with larger ones after 6 to 24 months—a method considered safer and more straightforward.
View photos of the appearance of the scrotum immediately following Phalloplasty and Scrotoplasty by Dr. Mang Chen and Dr. Walter Lin. Note: These are graphic operating room photos.
That said, some experienced surgeons still use tissue expanders when appropriate. Dr. Toby Meltzer, a leading gender-affirming surgeon in the U.S., has continued to use this technique. In his 2020 article "Metoidioplasty using labial advancement flaps for urethroplasty," he outlines the use of expanders as part of his staged approach to achieving optimal scrotal volume and aesthetics.
Tissue expanders have been used to enlarge the scrotum prior to implantation of testicular prostheses. Regardless of the timing of scrotal construction, placement of implants or tissue expanders is delayed for three months after the metoidioplasty to allow the neourethra to heal well without external pressure. If the scrotoplasty is performed as a secondary procedure, then the testicular implants or scrotal expanders can be placed at this time. Two weeks after implantation, the patient starts inflating them at home using 1-2 mL every other day. Expansion is stopped at 50 mL total in most cases. At least one month after completion of expansion, the permanent testicular implants are placed. The tubing from the expanders has been exteriorized on the mons with a two-way valve in response to some issues with compliance and irritation.
Other surgeons who sometimes use expanders include Dr. Curtis Crane and Dr. Dany Hanna.
Common Complications
As with any surgical procedure, scrotoplasty can involve certain risks and complications. The most common issues include:
- Minor wound separation (wound dehiscence):
The most frequent open wound occurs behind the scrotum, at the junction with the perineum. These wounds are usually small and shallow. With proper wound care they often heal on their own. - Fistula at the perineoscrotal junction:
In some cases, the wound described above may develop into a fistula, which is a small abnormal connection between tissues that can cause urine leakage. Depending on the severity, it may be managed conservatively or require surgical repair. - Partial flap tissue death (necrosis)
- Scrotum positioned too far back between the legs
- Scrotum too small to accommodate implants
- Loss of sensation due to nerve injury
When the scrotum heals too far back between the legs, a Monsplasty can be performed to reposition it. This procedure lifts the scrotum by reducing the fatty tissue over the mons pubis and helps bring the scrotum forward into a more typical position. It’s particularly helpful for patients with a prominent mons and is usually done about six months after the initial surgery. Monsplasty is a relatively low-risk, one-hour procedure and can be performed alongside testicular implant or penile implant placement.
If Monsplasty isn’t suitable, a scrotal lift is another option. This involves making incisions in the perineum and scrotum and advancing the tissue forward. However, the area must fully heal before testicular implants can be placed.
Hoebeke’s V-Y Scrotoplasty remains the gold standard for scrotal creation in gender-affirming surgery for its aesthetic, sensory, and functional outcomes. Additional procedures, such as the use of tissue expanders, monsplasty, and scrotal lifts, can further optimize results.
References
- Sengezer M, Sadove RC. Scrotal construction by expansion of labia majora in biological female transsexuals. Ann Plast Surg. 1993 Oct;31(4):372-6. doi: 10.1097/00000637-199310000-00016. PMID: 8239440.
- Hage JJ, Bouman FG, Bloem JJ. Constructing a scrotum in female-to-male transsexuals. Plast Reconstr Surg. 1993 Apr;91(5):914-21. doi: 10.1097/00006534-199304001-00029. PMID: 8460195.
- Selvaggi G, Hoebeke P, Ceulemans P, Hamdi M, Van Landuyt K, Blondeel P, De Cuypere G, Monstrey S. Scrotal reconstruction in female-to-male transsexuals: a novel scrotoplasty. Plast Reconstr Surg. 2009 Jun;123(6):1710-1718. doi: 10.1097/PRS.0b013e3181a659fe. PMID: 19483569.
- Miller TJ, Chen ML, Lin WC, Safa B, Watt AJ. Labia Majora Flap Scrotoplasty and Perineal Reconstruction in Phalloplasty Patients: Technique and Outcomes. Plast Reconstr Surg Glob Open. 2019 Sep 10;7(8 Suppl ):82-83. doi: 10.1097/01.GOX.0000584684.31625.6c. PMCID: PMC6750540.
- Meltzer TR, Esmonde NO. Metoidioplasty using labial advancement flaps for urethroplasty. Plast Aesthet Res. 2020;7:61. http://dx.doi.org/10.20517/2347-9264.2020.122
- Pigot GL, Al-Tamimi M, van der Sluis WB, Ronkes B, Mullender MG, Bouman MB. Scrotal Reconstruction in Transgender Men Undergoing Genital Gender Affirming Surgery Without Urethral Lengthening: A Stepwise Approach. Urology 2020 Dec;146:303. doi: 10.1016/j.urology.2020.09.017. Epub 2020 Sep 24. PMID: 32980404.
- Miller TJ, Lin WC, Safa B, Watt AJ, Chen ML. Transgender Scrotoplasty and Perineal Reconstruction With Labia Majora Flaps: Technique and Outcomes From 147 Consecutive Cases. Ann Plast Surg. 2021 Sep 1;87(3):324-330. doi: 10.1097/SAP.0000000000002602. PMID: 34397521.
Last updated: 06/03/25